Precision medicine is finally delivering on its promise, and the implications are profound
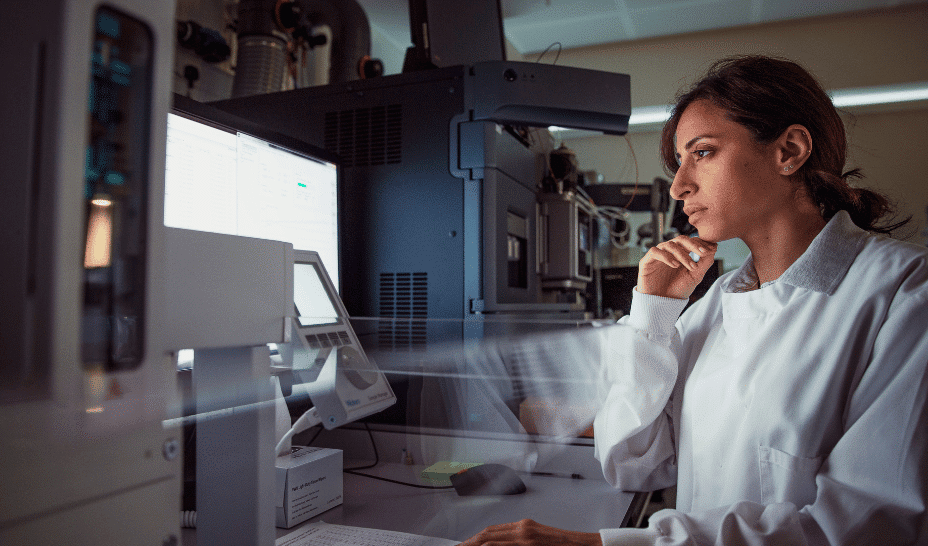
For decades, precision medicine has been more of an aspiration than a reality, a vision of tailoring treatments to the unique biology of each patient. Today, thanks to advances in data generation and computational power, this vision is turning into actionable breakthroughs at an unprecedented pace.
The challenge: vast amounts of data and how to structure it
One of the most significant shifts driving this progress is the ability to generate and interpret vast, multidimensional datasets at the cellular level. With the paradigm shift of AI, the ability to generate and capture vast amounts of data has had a horizontal impact, across multiple industries. In the scientific research sector, modern sequencing technologies now routinely produce terabytes of data from a single patient. That level of resolution means researchers can map pathogen heterogeneity, or in the case of Cure51, tumour heterogeneity, immune cell composition, and molecular signatures with a detail unimaginable just a few years ago.
Data alone, however, is not transformative without the capacity to analyse it. Until recently, the bottleneck in precision medicine was computational: no matter how much data you could generate, extracting patterns and insights required months or years of effort. Today, accelerated computing platforms and scalable AI frameworks are redefining what is possible. Workflows that once took weeks can now be accomplished in hours, and possibly soon in minutes. Complex modelling that was reserved for small pilot projects can finally scale across thousands of patients. This combination of high-fidelity data and industrial-strength analytics is the foundation of a new era of medical discovery.
What precision medicine means for cancer research
The impact is already visible in oncology. By integrating single-cell sequencing, spatial transcriptomics, and imaging data, researchers are beginning to identify survival-associated signatures that would be impossible to detect in aggregate population studies alone. These signals are helping to redefine how we classify disease subtypes, predict patient outcomes, and prioritise therapeutic targets. They also highlight an important philosophical shift: moving from studying disease progression in average patients to understanding exceptional outcomes in individual cases.
Consider, for example, the long-overlooked phenomenon of patients with advanced cancer who survive far beyond statistical expectations, which is what we are looking at in particular. These exceptional responders have often been labelled as outliers and essentially deemed too rare to inform broader therapeutic strategies. Yet with the tools we have today, their biology becomes a roadmap. If you can systematically catalogue and analyse the molecular and cellular environments of these patients, you can start to see patterns that explain why some immune systems succeed where others fail. These insights have the potential to unlock new drug targets and predictive biomarkers that improve care for all patients, not just the fortunate few.
Precision medicine: a light at the end of the tunnel for chronic diseases
The same combination of rich data and advanced analytics is now driving progress in autoimmune diseases, neurodegenerative disorders, and rare diseases. In each case, we are witnessing the convergence of disciplines such as genomics, proteomics, digital pathology, and computational biology into integrated platforms that learn and improve over time. This convergence is not theoretical. It is already delivering real results: shorter development timelines, better patient stratification, and more efficient clinical trials.
What’s equally exciting is how this transformation is democratising discovery itself. Historically, only the largest research institutions and pharmaceutical companies had the resources to work with datasets of this scale. Today, cloud-based computing infrastructure and AI-powered pipelines are putting these capabilities into the hands of smaller research teams and innovative biotech companies. As a result, the barriers to entry for high-impact precision medicine are coming down, and the pace of innovation is accelerating.
Still, the future of precision medicine will depend on more than technology alone. It requires a new mindset, one that values patient diversity, longitudinal data collection, and collaboration across disciplines. It also requires sustained investment in building the infrastructure and partnerships that make this work possible at scale.
The opportunity ahead of us is enormous. We have a chance to fundamentally redefine how we understand disease and develop therapies, not based on averages, but on the nuanced reality of individual biology. For patients and clinicians, this means treatments that are not only more effective but also more personal. For researchers and entrepreneurs, it means a once-in-a-generation opportunity to translate complexity into cures. Precision medicine has been a promise for too long. Today, it is finally becoming a practice, and the implications for human health are immense.
The post Precision medicine is finally delivering on its promise, and the implications are profound appeared first on EU-Startups.