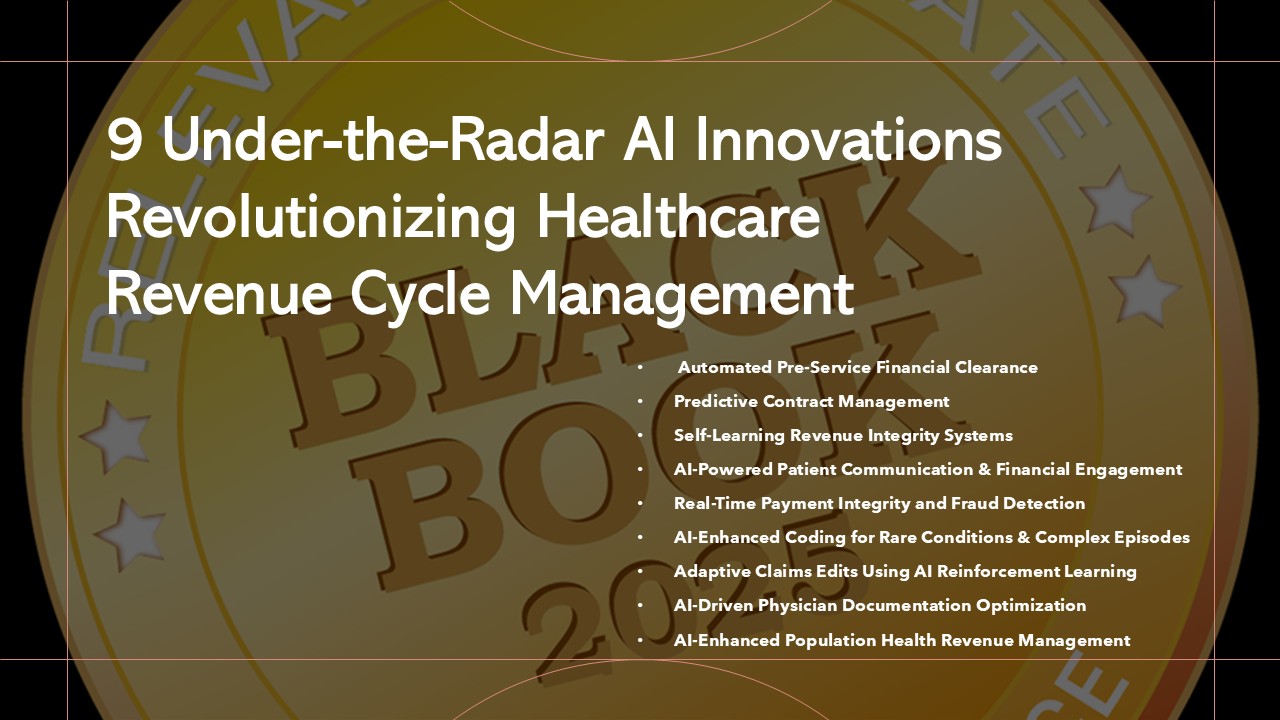
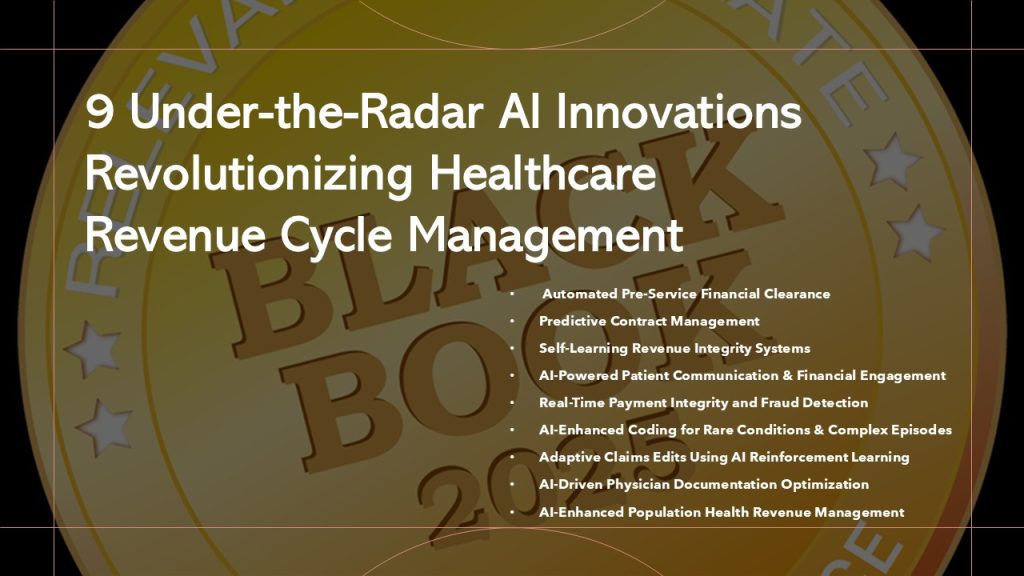
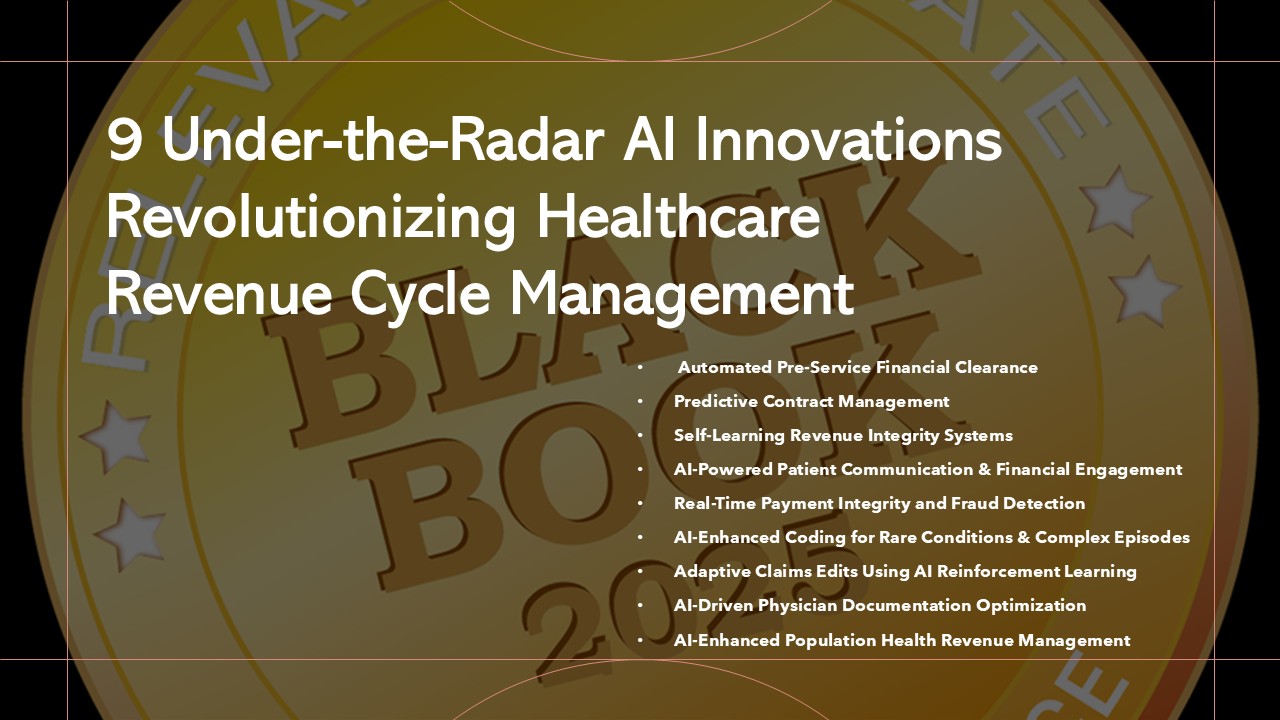
9 Under-the-Radar AI Innovations Set to Transform Healthcare Revenue Cycle Management- Black Book Research
New Survey Uncovers Hidden AI Solutions Delivering Major Provider Gains in Efficiency, Accuracy, and Patient Experience
NASHVILLE, TENNESSEE / ACCESS Newswire / April 21, 2025 / Artificial intelligence (AI) continues to reshape healthcare, with significant yet lesser-known advancements emerging specifically within Revenue Cycle Management (RCM). Black Book Research’s independent study from Q2 2025 surveyed 460 revenue cycle professionals across hospitals, physician groups, diagnostic centers, and long-term care facilities, revealing impactful but under-the-radar AI innovations. These technologies are driving notable improvements in operational efficiency, financial accuracy, and patient engagement.
A notable insight from the Black Book survey indicates that while mainstream media focuses heavily on clinical AI applications, nearly 80% of RCM professionals believe these underreported AI-driven financial technologies are critical to their organizations’ success. Doug Brown, Founder of Black Book Research, noted, “Our research uncovered substantial opportunities within AI capabilities that aren’t often discussed publicly. Healthcare providers leveraging these under-the-radar innovations report significant operational and financial improvements, underscoring their vital role in today’s rapidly evolving healthcare landscape.”
The following nine AI innovations, ranked highly by professionals in the field, provide transformative capabilities:
1. Automated Pre-Service Financial Clearance AI solutions manage patient financial responsibilities proactively by predicting expenses, verifying insurance, and preventing claim denials before services are provided.
AI RCM Vendor Names by Respondents: Waystar, Optum360, R1 RCM
Startup Vendors to Watch: qBotica, Alpha Health, TailorMed
____________
Survey Insight: Ranked top innovation by 78%; 85% reported improved upfront collections and reduced denials.
2. Predictive Contract Management Machine learning analyzes payer contracts comprehensively, identifying discrepancies and proactively resolving underpayments pre-submission.
AI RCM Vendor Names by Respondents: Rivet Health, FinThrive, Enter.Health
Startup Vendors to Watch: AKASA, Anomaly, HealthTensor
Survey Insight: Ranked top three by 71%; 80% noted fewer reimbursement issues and enhanced revenue accuracy.
____________
3. Self-Learning Revenue Integrity Systems AI systems continuously analyze historical and real-time billing data, refining billing accuracy and documentation to minimize repeated denials.
AI RCM Vendor Names by Respondents: MediCodio, AGS Health, Thoughtful AI
Startup Vendors to Watch: SmarterDx, Fathom, Robin Healthcare
Survey Insight: Highly rated by 74%; 83% cited significant reduction in denials and improved compliance.
____________
4. AI-Powered Patient Communication and Financial Engagement Conversational AI proactively engages patients regarding financial responsibilities, enhancing patient satisfaction and improving collections.
AI RCM Vendor Names by Respondents: Collectly, RevSpring, Experian Health
Startup Vendors to Watch: Inbox Health, Cedar, MedPilot
Survey Insight: Highlighted by 69%; 78% reported improved payment rates and patient satisfaction.
____________
5. Real-Time Payment Integrity and Fraud Detection AI monitors claims in real-time, swiftly detecting fraud, waste, and compliance anomalies, significantly enhancing payment integrity.
AI RCM Vendor Names by Respondents: Codoxo, SAS, MultiPlan
Startup Vendors to Watch: Clarify Health, Fraudscope, Protenus
Survey Insight: Recognized by 76%; 82% noted increased accuracy and reduced fraud incidents.
____________
6. AI-Enhanced Coding for Rare Conditions and Complex Episodes Specialized NLP and machine learning accurately code complex medical scenarios, reducing coding errors, denials, and appeals.
AI RCM Vendor Names by Respondents: MediCodio, RapidClaims, CareCloud’s cirrusAI
Startup Vendors to Watch: Nym Health, Suki AI, ForeSee Medical
Survey Insight: Valued by 70%; 77% experienced fewer errors and improved reimbursement accuracy.
____________
7. Adaptive Claims Edits Using AI Reinforcement Learning AI dynamically adjusts claim editing workflows based on payer behaviors, improving claim acceptance and reducing manual adjustments.
AI RCM Vendor Names by Respondents: Availity, Thoughtful AI, Waystar
Startup Vendors to Watch: Digitize.AI, Curation Health, PayrHealth
Survey Insight: Emphasized by 68%; 80% observed higher claim acceptance rates and reduced processing times.
____________
8. AI-Driven Physician Documentation Optimization Real-time AI feedback during clinical documentation ensures accuracy, completeness, and compliance, improving clinician satisfaction.
AI RCM Vendor Names by Respondents: Microsoft’s Dragon Copilot, Navina, Abridge
Startup Vendors to Watch: Augmedix, DeepScribe, ScribeEMR
Survey Insight: Highly rated by 72%; 84% reported improved clinician satisfaction and reduced documentation denials.
____________
9. AI-Enhanced Population Health Revenue Management AI integrates population health management with financial workflows, offering predictive analytics for risk management, reimbursement optimization, and quality-based financial forecasting.
AI RCM Vendor Names by Respondents: Innovaccer, Health Catalyst, Arcadia
Startup Vendors to Watch: Apixio, Socially Determined, ClosedLoop.ai
Survey Insight: Recognized by 73%; 81% reported improved financial outcomes aligned with population health goals.
Strategically adopting these innovative AI technologies enables healthcare providers to achieve substantial operational and financial improvements, securing a strong competitive position in the evolving healthcare landscape.
___________
About Black Book Research Healthcare RCM AI Innovation Category
% Ranked Top/Top 3
% Reported Key Outcome
Automated Pre-Service Financial Clearance
78%
85% improved upfront collections/reduced denials
Predictive Contract Management
71%
80% fewer reimbursement issues/enhanced accuracy
Self-Learning Revenue Integrity Systems
74%
83% reduction in denials/improved compliance
AI-Powered Patient Communication & Engagement
69%
78% improved payment rates/patient satisfaction
Real-Time Payment Integrity & Fraud Detection
76%
82% increased accuracy/reduced fraud
AI-Enhanced Coding for Rare/Complex Episodes
70%
77% fewer errors/improved reimbursement
Adaptive Claims Edits Using AI
68%
80% higher claim acceptance/reduced processing time
AI-Driven Physician Documentation Optimization
72%
84% improved clinician satisfaction/reduced denials
AI-Enhanced Population Health Revenue Management
73%
81% improved financial outcomes
Black Book Research is a premier source for unbiased, independent research in healthcare technology and services. Each year, Black Book publishes industry-leading reports and resources designed to help healthcare professionals stay informed about the latest trends and innovations. The upcoming 2025 Black Book of Healthcare Revenue Cycle Management Solutions is an annual updated resource that provides comprehensive insights, rankings, and guidance to assist healthcare organizations in making informed RCM decisions.
Contact Information
Press Office
[email protected]
8008637590
SOURCE: Black Book Research
View the original press release on ACCESS Newswire
The post 9 Under-the-Radar AI Innovations Set to Transform Healthcare Revenue Cycle Management- Black Book Research appeared first on European Business & Finance Magazine.